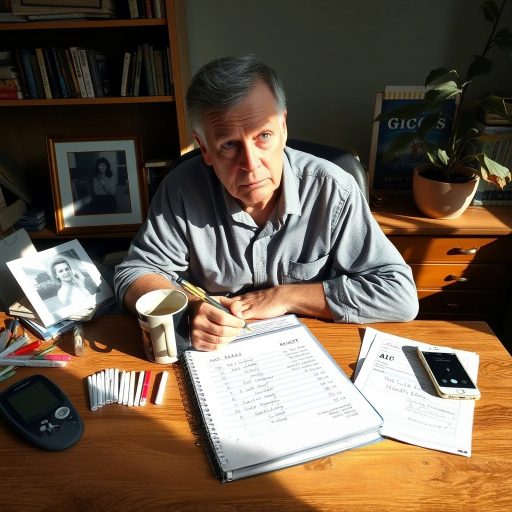
Let’s cut to the chase: managing blood sugar feels like playing a high-stakes game of Jenga while blindfolded, especially when converting blood sugar levels to A1C. You pull out one block (a glucose reading), and suddenly the whole tower wobbles (your A1C). But here’s the kicker—you’re not just building a tower; you’re navigating a labryinth of numbers that supposedly dictate your health fate. I get it. I’ve been there. Three years ago, my own A1C report made me feel like I’d failed some cosmic exam. Turns out? The system’s rigged—not against you, but against simplicity. Let’s untangle this mess.
The Blood Sugar-A1C Tango: Why Your Numbers Feel Like a Foreign Language
Picture this: You’re logging glucose readings like a champ—140 mg/dL fasting, 180 after dinner—and patting yourself on the back. Then your A1C comes back at 7.2%, and suddenly you’re questioning everything. Did I log wrong? Am I a failure? (Spoiler: No, but the system’s designed to make you feel that way.)
A1C measures the sugar-coating on your red blood cells over ~90 days. It’s like taking a 3-month average of your relationship status—it’s not exactly the whole story, but it gives a vibe. The formula? Roughly: A1C (%) ≈ (Average Blood Sugar + 46.7) ÷ 28.7. But here’s the thing: this math assumes your body behaves like a textbook. Spoiler alert—it doesn’t.
The Risks of Being Too “Perfect” With Numbers
Here’s where it gets wild. I once met a guy who swore his fasting glucose was “perfect” at 85 mg/dL. But his post-meal spikes hit 300 like it was his job. His A1C? 8.5%. The kicker? He thought he was “fine” because his fasting numbers were “normal.” Turns out, A1C doesn’t care about your fasting ego—it wants the average, including those post-pasta meltdowns.
Ignoring this? It’s like driving a car while only checking the speedometer once a day. Sure, you might think you’re cruising at 60 mph, but what if you’re actually swerving between 30 and 100? That’s blood sugar volatility—and it’s a beast A1C subtly hints at but never fully explains.
The Formula: A Clunky but Useful Tool
Alright, let’s get practical. To convert blood sugar to A1C:
- Find Your Average: Track 7–14 days of readings (fasting, post-meal, random). Add ’em up, divide by the count.
- Plug Into the Equation: Let’s say your average is 180 mg/dL. (180 + 46.7) ÷ 28.7 ≈ 7.9%.
- Compare to Lab Results: If your calculated A1C clashes with the lab’s, something’s off. Maybe your RBCs are retiring early (thanks, anemia!), or you’re a genetic outlier.
Pro tip: Use apps like Dexcom or MySugr—they’re like having a co-pilot who’s obsessed with spreadsheets.
Why Your A1C Might Be a Hot Mess
Let’s talk limitations. A1C isn’t a crystal ball—it’s more like a foggy window. Factors that screw it up:
- Short RBC lifespan: Kidney disease, anemia, or hemolytic disorders? A1C lies.
- Extreme variability: If your glucose swings from 50 to 400 daily, A1C averages out the chaos—but your body feels those swings.
- Genetic quirks: Some folks have weird hemoglobin variants. Labs call this “HbA1c interference.” You call it “bullshit.”
Real talk: If your home calculations and lab results clash, dig deeper. Ask for a fructosamine test—it’s like A1C’s shorter-term cousin (2–3 weeks).
Turning Numbers Into Action: Because Data Alone Won’t Fix You
Okay, so you’ve calculated your A1C. Now what? Here’s where the rubber meets the road—and where most guides ghost you.
- Set Goals That Don’t Suck: Aim for a 0.5–1% drop in 3 months. Smaller steps = sustainable wins.
- Track Patterns, Not Just Numbers: Notice how tacos spike you? Swap the rice for a salad. Obvious, right? But doing it? That’s the struggle.
- Use Tech, But Don’t Worship It: CGMs like Freestyle Libre are genius—but they’re not therapists. They’ll show you trends, but you have to care enough to act.
Personal rant: Why is this so damn hard? Because health isn’t a math problem—it’s a lifestyle puzzle with emotional tax.
FAQs: Because You’re Probably Still Confused
Q: How often should I check my A1C?
A: Every 3–6 months, depending on whether you’re newly diagnosed, adjusting meds, or just cruising.
Q: Can I lower my A1C fast?
A: Yes, but rapid drops (like 2% in a month) usually mean extreme dieting or stress. Neither’s fun long-term.
Q: Is A1C the only metric that matters?
A: Hell no. Time-in-range (from CGMs) and post-meal spikes tell a fuller story. A1C’s just the cliffnotes.
The Bottom Line: Embrace the Chaos, Then Take Control
Managing blood sugar isn’t about perfection—it’s about progress. Your A1C is a clue, not a verdict. Calculate it, compare it, then get curious. Why is it what it is? What can you tweak? And remember: You’re not alone in this.
I’ll leave you with this: Last week, a patient told me, “My A1C dropped 1.5% in 90 days, and I didn’t even try that hard.” How? She swapped soda for sparkling water and walked 10 minutes after meals. Small changes, big impact.
Your turn. Calculate. Reflect. Adjust. And for heaven’s sake, be kind to yourself.
