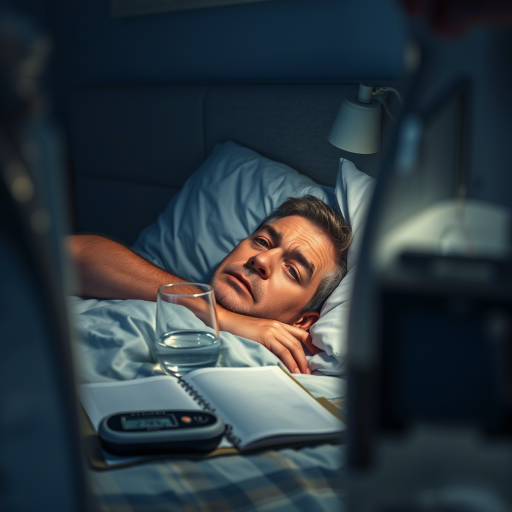
Introduction: The Hidden Danger of High Blood Sugar at Night
If you’ve ever woken up feeling exhausted despite a full night’s sleep, or noticed frequent trips to the bathroom after dark, you might be experiencing nocturnal hyperglycemia—elevated blood sugar levels during sleep. This silent disruptor affects millions with diabetes or prediabetes, yet it often goes unnoticed until complications arise. Left untreated, it can lead to nerve damage, cardiovascular risks, and relentless fatigue. But with the right strategies, you can regain control. This guide reveals the most effective, science-backed methods to identify, manage, and prevent nighttime blood sugar spikes.
Recognizing the Symptoms of High Blood Sugar at Night
Key Indicators You Can’t Ignore
- Frequent Nighttime Urination (Nocturia): Elevated glucose pulls fluid from tissues, causing urgent bathroom visits.
- Thirst and Dry Mouth: High blood sugar dehydrates the body, triggering relentless thirst.
- Fatigue and Headaches: Poor sleep quality from interrupted rest leaves you drained.
- Blurred Vision: Fluctuating glucose levels impair vision clarity.
- Unexplained Weight Loss: Insulin resistance burns muscle instead of fat.
Subtle Signs Often Overlooked
- Restless Sleep: Night sweats or tossing may signal glucose swings.
- Morning Dizziness: Low blood sugar after a spike (rebound hypoglycemia) causes lightheadedness.
- Increased Hunger: Poor nutrient absorption leaves you ravenous.
Why Nocturnal Hyperglycemia Happens—and How to Fix It
The Dawn Phenomenon
Your body naturally releases cortisol and growth hormone at dawn, raising glucose levels. Pair this with insulin resistance, and nocturnal spikes are inevitable.
The Somogyi Effect
Low blood sugar overnight triggers hormone surges that overcorrect, causing morning highs. Monitor glucose trends to differentiate.
Q&A: Why Does Blood Sugar Rise at Night?
Q: Is nighttime snacking the culprit?
A: Not always. Carbs before bed spike glucose, but cortisol and insulin resistance play bigger roles.
The Gold Standard Strategies for Management
Dietary Adjustments
- Carb Timing: Eat complex carbs (quinoa, lentils) earlier in the day.
- Protein and Fiber: Snack on almonds or Greek yogurt to stabilize glucose.
- Avoid Sugar Spikes: Skip sugary desserts post-dinner.
Blood Sugar Monitoring
- Continuous Glucose Monitors (CGMs): Track real-time trends to spot nocturnal spikes.
- Fasting Tests: Measure morning glucose to assess overnight control.
Medication and Insulin
- Extended-Release Metformin: Reduces liver glucose production overnight.
- Basal Insulin Adjustments: Consult your doctor to fine-tune doses.
Prevention: A Supreme, Proven Approach
Exercise Timing
- Evening workouts improve insulin sensitivity but avoid intense activity 2 hours before bed.
Stress Management
- High cortisol exacerbates glucose spikes. Try meditation or yoga before sleep.
Consistent Sleep Schedule
- Poor sleep disrupts hormones. Aim for 7–9 hours nightly.
When to Seek Help
Red Flags
- Repeated morning glucose >180 mg/dL.
- Symptoms like confusion, nausea, or rapid heartbeat.
Q&A: When Should I Call My Doctor?
Q: My blood sugar is 200 mg/dL at midnight. Is this an emergency?
A: If you’re asymptomatic, monitor. Persistent highs require medical review.
The Most Comprehensive Action Plan
- Track Glucose Trends: Use a log or CGM to identify patterns.
- Optimize Dinner: Prioritize protein and non-starchy veggies.
- Stay Hydrated: Water thins blood, aiding glucose transport.
- Review Medications: Certain drugs (steroids, antipsychotics) raise glucose.
- Educate Yourself: Attend diabetes workshops or join support groups.
Conclusion: Your Path to Better Sleep and Health
Nocturnal hyperglycemia isn’t inevitable. With vigilant monitoring, strategic diet tweaks, and lifestyle adjustments, you can reclaim restful nights. Start small—swap a bedtime cookie for a handful of nuts, or set a reminder to check glucose at midnight. Every step toward stability reduces long-term risks.
Ready to take control? Drop your email above to bust type 2 diabetes by activating cells for stable blood sugar. Or schedule a telehealth visit with an endocrinologist to personalize your strategy.
